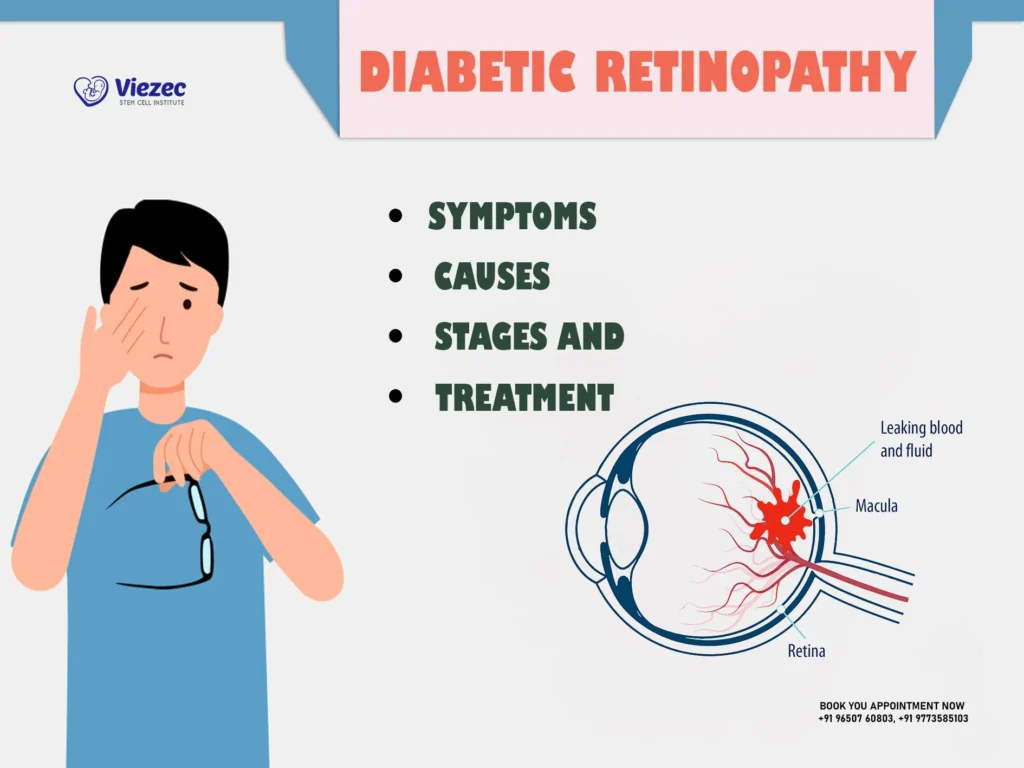
Diabetic retinopathy is a progressive eye disease caused by high blood sugar levels damaging the small blood vessels in the retina. The retina plays a crucial role in vision by capturing light and sending signals to the brain. When its blood vessels weaken, they may swell, leak, or become blocked, leading to vision problems. If left untreated, diabetic retinopathy can cause permanent blindness.
Symptoms of Diabetic Retinopathy
Many people with diabetic retinopathy do not experience noticeable symptoms in the early stages. As the condition worsens, vision may become blurry or fluctuate. Floaters, which appear as dark spots or strings in the field of vision, can also increase. Some people struggle to see at night or notice that colors appear faded. In more advanced cases, dark areas may develop in the vision, or complete vision loss can occur. Because these symptoms progress gradually, regular eye exams are the best way to detect the disease early.
Stages of Diabetic Retinopathy
Diabetic retinopathy develops in four stages. In the mild nonproliferative stage, tiny bulges form in the blood vessels of the retina, but vision remains mostly unaffected. As the disease progresses to moderate nonproliferative retinopathy, some blood vessels become blocked, reducing oxygen flow and causing mild visual disturbances. In the severe nonproliferative stage, the damage increases, and the retina starts signaling the body to grow new blood vessels. This leads to proliferative diabetic retinopathy, the most advanced stage.
How is Diabetic Retinopathy Diagnosed?
Annual eye exams are crucial for diagnosing diabetic retinopathy before symptoms appear. The most effective method is a dilated eye exam, in which an eye doctor uses special drops to widen the pupils and examine the retina for signs of damage. Retinal photography is another diagnostic tool that captures high-resolution images of the retina to detect abnormalities. Optical coherence tomography (OCT) provides detailed cross-section images of the retina to check for swelling or other changes. If dilation is not an option, retinal imaging can be used as an alternative, but it should always be reviewed by an eye specialist to ensure accuracy.
Treatment Options for Diabetic Retinopathy
Treatment depends on the severity of the disease. In the early stages, no immediate intervention may be necessary. Instead, managing blood sugar, blood pressure, and cholesterol levels can help slow its progression. However, in advanced cases, medical treatments are required.
One common approach is the use of anti-VEGF injections, which reduce the growth of abnormal blood vessels and prevent swelling in the retina. Another option is laser therapy, also known as photocoagulation, which seals leaking blood vessels and stops further damage. In severe cases where there is significant bleeding or scar tissue formation, a vitrectomy may be necessary. This surgical procedure removes blood and debris from the eye to restore vision. Early treatment greatly improves the chances of preserving eyesight.
Can You Prevent Diabetic Retinopathy?
While diabetic retinopathy cannot always be prevented, certain lifestyle changes can significantly reduce the risk. Keeping blood sugar levels stable is the most effective way to protect eye health. A balanced diet, as well as regular exercise, and prescribed medications can help maintain healthy glucose levels. Controlling blood pressure and cholesterol is equally important, as high levels can contribute to blood vessel damage in the retina. Smoking increases the risk of vision problems, so quitting can help prevent complications.
Living with diabetic retinopathy disease
Managing diabetic retinopathy requires ongoing care and attention to eye health. If vision changes occur, using magnifiers, high-contrast screens, and adequate lighting can help with daily activities. Seeking support from low-vision specialists and joining support groups can provide helpful strategies for coping with vision impairment.
